For such a well-known condition, MS is difficult to pin down, as Neil Hartigan explains.
Multiple sclerosis (MS) is a disease of the central nervous system. Fibres in the nervous system are covered with a substance called myelin, which acts as an insulator and allows impulses to travel down the nerves quickly and efficiently.
In MS, the myelin becomes inflamed and scarred, and is eventually destroyed: sometimes MS is referred to as demyelination for this reason.
Nerve impulses become weaker as the myelin becomes less efficient, and may eventually fail altogether. Whatever is being controlled by the affected nerve will therefore also become weaker and unable to respond to the signals from the brain.
About 100,000 people in the UK have MS, usually diagnosed in people between the ages of 20 and 40, and it affects roughly three times as many women as men. The cause is not fully understood and there is no cure. Once diagnosed, MS stays with you for life, but treatments and specialists can help to manage the condition and its symptoms.
Signs and Symptoms
Physical symptoms of MS might commonly include: visual problems, balance problems and dizziness, fatigue, bladder problems and stiffness or spasms. Other symptoms may include problems with: bowel, speech, swallowing and tremor. MS can also affect memory and thinking, and may have an impact on emotions.
Diagnosis and Tests
As MS is complex and as it can cause many different symptoms, it is not easy to diagnose. It is hard to pinpoint exactly when MS begins, and the early signs and symptoms are different from person to person.
It is not unusual for a diagnosis to take several months or even longer. There are many tests a Neurologist will use to find out if someone has MS, but there is no single definitive test to determine a diagnosis. While negative testing makes a diagnosis of MS less likely, it does not rule it out.
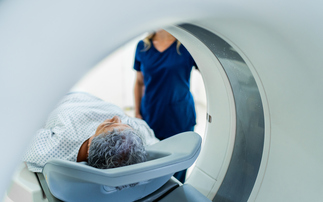
Currently, the most reliable test is MRI (magnetic resonance imaging) scanning of the brain and spinal cord. Areas of demyelination show up as white plaques, and more than 90% of people with MS will have MRI scans that are positive for plaques.
Another test usually carried out is an investigation for proteins in the cerebrospinal fluid, known as oligoclonal banding, through a lumbar puncture, which can be painful.
A totally painless and non-invasive test is ‘evoked responses', where the patient is wired to an encephalogram and the brain activity response to stimuli such as flashing lights is measured. MS is indicated by the time it takes for these messages to get through to the brain.
While there is actually no standard clinical set of rules for the diagnosis of MS, it is usually based on a series of guidelines called the McDonald criteria, which state that the symptoms must be disseminated in space (ie, more than one set of symptoms) and time (ie, more than one event).
The symptoms must have lasted for more than 24 hours, and to qualify for being more than one event they must be 30 days apart. The McDonald criteria are also heavily dependent on MRI results.
Various combinations of events in time, space and positive MRI results will lead to a diagnosis of MS, although this is by no means clear cut, especially in the early stages of the disease. This can create problems when underwriting.
There are 79 conditions that mimic MS. Diagnostic evaluation strategies used to rule out alternative diagnoses depend on the following
- Where clinical, laboratory and imaging results are classic features of MS with no strong features of an alternative diagnosis, no further tests will be carried out;
- Where features are compatible with MS but are also red flags for other conditions, tests are required to exclude alternative diagnoses;
- If there are red flags that point to an alternative diagnosis and MS is improbable, an alternative diagnosis will be looked for.
Types of MS
There are four main sub-types of MS, the classification of which depends on the clinical course following diagnosis.
Relapsing remitting
About 85% of people with MS have this type. There are unpredictable periodic relapses, with interim periods of remission that may last months or years. During the attacks, the disease activity causes symptoms of visual, sensory and motor disturbances that may resolve during remission, or may be permanent to some degree.
Where they are permanent, each relapse will leave the patient with increasingly impaired neurological function. A small number of people will have very long periods of remission with small relapses and complete recovery in between. This type is often referred to as ‘benign' MS, but can only be described as such when this clinical course has been followed for ten years.
Secondary progressive
This is where there is a relapsing-remitting onset, but after a period of time there is a steady deterioration in neurological function with no periods of remission. About 50% of people with relapsing-remitting MS will go into the secondary progressive phase after 15 years. The decline may include new neurological symptoms, worsening cognitive function or other deficits. Secondary progressive causes the greatest degree of disability.
Primary progressive
About 10% of those diagnosed with MS have this type. The initial symptoms have an insidious and vague onset, followed by a steady decline in function with no periods of remission. Typically, the age of onset is later, commonly at about 40 years of age. In severe cases, disability occurs within five years of the initial symptoms.
Progressive relapsing
This is the least common subtype which begins with a progressive course, but periodic attacks do occur as well.
Treating MS
At present, there is no cure for MS, and treatment is dependent on the type of disease and typically falls into three categories:
- Treatment that modifies the course of the disease;
- Treatment that affects the severity and duration of a relapse;
- Symptomatic treatment or rehabilitation.
Immunosuppressive therapy is used to modify the course of the disease. The following medications slow its course and inhibit the accumulation of plaque:
- Interferon beta;
- Glatiramer acetate;
- Methotrexate;
- Corticosteroids (which are used to treat relapses).
Symptomatic treatment depends on symptoms. Treatment for spasticity can include:
- Baclofen;
- Dantrolene;
- Diazepam.
Anti-depressants or antivirals may be prescribed for symptoms of fatigue.
Management of the disease can be complimented through the use of exercise, diet and physiotherapy.
Underwriting Considerations
With a condition so difficult to diagnose, incurable, and with a very varied, unpredictable course, it is not surprising that the underwriting outcome is also extremely varied. Terms can be anything from standard rates for benign MS to decline where progression has been rapid. Critical illness will ordinarily be declined if a diagnosis of MS has been made.
Generally, terms are only available for the relapsing-remitting type of MS. An underwriting assessment is typically made using the criteria below:
- Type of MS;
- Date of diagnosis;
- Details of any neurological episodes prior to diagnosis;
- Symptoms and course since diagnosis;
- Treatment;
- Current neurological status;
- Degree of disability where present;
- Complications;
- Progression.
Assessment can take into account good prognostic indicators such as:
- Onset < 25;
- Relapsing remitting onset;
- Sensory symptoms (numbness/optic neuritis);
- Complete recovery between relapses;
- Infrequent relapses;
- Few attacks early in course (less than four in two years);
Long time to permanent disability.
Or poorer prognostic features such as:
- Onset > 40;
- Motor symptoms;
- Incomplete recovery between relapses;
- Frequent relapses;
- Many attacks early in course (within 6 months);
- Short time to permanent disability.
One of the biggest issues for underwriters is assessing a case where MS is suspected but not diagnosed, particularly when critical illness has been applied for.
Where there is a disclosure of vague neurological symptoms, such as pins and needles/tingling, numbness, blurred vision, bladder dysfunction, tremor, weakness and fatigue, and others, it may mean that critical illness is declined, or multiple sclerosis is excluded.
For critical illness, family history is significant and depending on the combination of sex and family members affected, an exclusion may be applied.
Neil Hartigan is underwriting and development manager at PruProtect